Mental Health Awareness Week
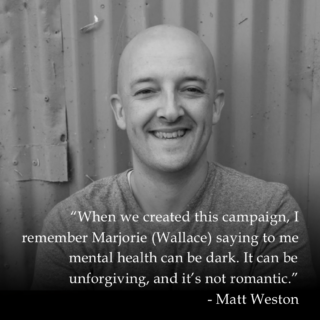
The theme of Mental Health Awareness Week (May 9-15) this year is loneliness, and while some people say they have been isolated but not lonely over the last two years, for others the combination has left them feeling exposed and desperate.
Even with lockdown restrictions lifted, many people still feel alone. SANE’s concern is that when people do reach out for help, it is mostly non-existent.
Loneliness is often characterised by a sense of shame which can isolate someone even more than they already are, and a sense of frustration that they cannot connect in a meaningful way with people who are around them.
It can trap somebody in a downward spiral and can have a profound effect on a person’s mental and physical health.
Isolation
Weak social connections can have a similar impact on a person’s physical health as smoking, and we have become increasingly concerned about the escalating epidemic of depression, anxiety and self-harm amongst young people, particularly teenage girls. These conditions drive, and can be driven by, social isolation.
Everybody who calls our telephone helpline, SANEline, and uses our support services has experienced some degree of loneliness and isolation, and one of our aims is to help people feel less alone, even if only for the duration of the call.
The consequences of loneliness and isolation can be profound without some form of intervention and connection with other people.
Difficulty accessing inpatient care when in crisis – even when lucky enough to get a bed – patients are often sent miles from home. The Government pledged to end out-of-area placements by the end of 2020/2021, but recent figures show progress has stalled.
People are still being failed and left with nowhere to turn when in crisis. And it is not just in the NHS that safe effective care can sometimes be lacking.
Lack of beds
The reduction in specialist mental health beds in recent years and the Government’s failure to address this has left the NHS over-reliant on private sector providers.
It has been reported that increasing amounts of money is being spent by the NHS on private hospital placements. But even in the private sector there are problems.
As patients are transferred to providers sometimes away from family and support networks, safe, effective care can still be lacking as it is in the NHS.
Some providers have been highlighted by health watchdog the Care Quality Commission over standards of care, and a coroner recently highlighted his concerns following a deeply concerning tragedy.
The last two years have been challenging and mental health services experienced unprecedented demand from people struggling and seeking support.
Funding
The extra £2.3bn from Government for mental health services until 2024 is a start, but the proposed 10-year mental health plan, must lead to a service that is able to respond to individual needs at the time a person reaches out for help, or when they need consistent support.
Too many people still don’t know where to turn to for support or can’t access help early enough. We are concerned at the scale of the problem, with 500,000 people regularly going up to a week without seeing anybody at all in the UK.
Easing the burden on the seven million carers in the UK alone, the overwhelming majority of whom struggle with loneliness, will require huge effort and funding.